Cataracts, a natural result of the aging process, are the world’s leading cause of blindness. Although humans have known about cataracts for thousands of years, treatment options for most of our history were limited to painful and dangerous procedures that offered little in the way of visual improvement. Check out these interesting and little-known facts to learn more about the history of cataracts!
Cataract surgery has been performed for thousands of years.
The earliest artistic representation of a cataract is a small wooden statue of an Egyptian priest from approximately 2457-2467 B.C.E. A white patch, believed to represent a cataract, is carved into the priest’s left eye. The earliest known representation of a cataract removal procedure appeared on the walls of Egyptian temples and tombs centuries later. The word “Cataract” come from the Greek word used for “waterfall” because prior to the 1700s, people believed that cataracts were “opaque material flowing like a waterfall, into the eye”.
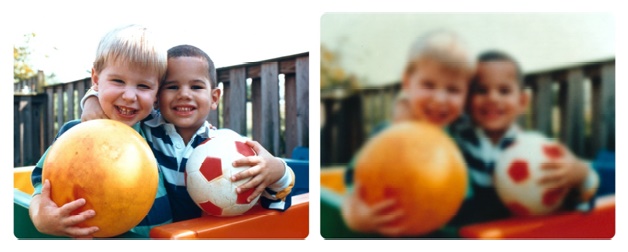
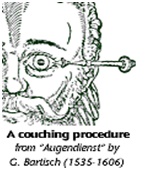
500 B.C a procedure, known as couching, could only be performed on people with advanced cataracts. As cataracts worsen, the lens becomes opaque and rigid and the lens capsule and zonules that hold it in place weaken. Early couching procedures involved hitting the patient’s eye with a blunt object in order to displace the lens so it could be absorbed into the vitreous humor in the back of the eye. Because contact lenses hadn’t been invented yet, patients were often left slightly improved but extremely blurry vision.
Early cataract surgery involved a needle, a steady hand, and no anesthetics.
Though cataract removal procedures remained relatively unchanged for centuries, by 29 AD Western physicians had started using a needle break to break up cataractous lens into smaller pieces that would be more easily absorbed into the back of the eye. Because topical anesthetics wouldn’t be more invented for a few hundred more years, doctors required the help of a strong-armed assistant to hold the patient down while they jabbed their eye with a needle. Ouch.
The advent of “needling” meant that patients did not have to wait until they had advanced cataracts to have them removed. However, as antibiotics and sterile surgical equipment were still a few centuries in the making, the procedure had a high mortality rate, a long recovery period, and still left patients with incredibly blurry vision.
Parisian Jacques Daviel performed the first cataract extraction procedure in 1748.
In couching and needling procedures, the lens was not actually removed from the eye – just displaced and reabsorbed. In Daviel’s procedure, an incision was made to the outer layer of the eye in order to completely remove the lens, leaving part of the lens capsule behind. Londoner Samuel Sharpe introduced a new variation of this surgery in 1753, in which he used his thumb to apply pressure and pop the lens out of the eye. Thankfully, by 1902, doctors were using small suction cups and forceps – you know, actual medical equipment – to remove the lens from the eye.
Intraocular lenses were first developed in 1940 by Englishman Harold Ridley.
Up until the invention of the intraocular lens, cataract surgery left patients with poor visual acuity. Although patients were no longer experiencing cloudy, yellowed, or distorted vision, the lack of lens made it impossible for their eyes to focus light. IOLS changed everything for cataract patients.
Made of plastic, early IOLs provided a permanent solution to vision loss associated with cataracts by giving the eye another lens through which to focus. This improved visual acuity in addition to getting rid of a patient’s cataracts. Since then, IOLs have received numerous upgrades to make them safer and more comfortable for wearers. Now, IOLs are made out of flexible material that respond to your eye muscle’s natural movements and can treat a number of eye problems, including presbyopia and astigmatisms.
In 1967, New Yorker Charles Kelman introduced the phacoemulsification technique for cataract surgeries.
Unlike previous procedures that required a large incision in the cornea to remove cataracts, this technique uses ultrasonic vibrations to break up the lens into incredibly small pieces that could be sucked out through a tiny incision in the eye. Kelman’s innovation, which was less painful and had a shorter recovery time than other cataract removal procedures, further improved the patient experience during and after the surgery.
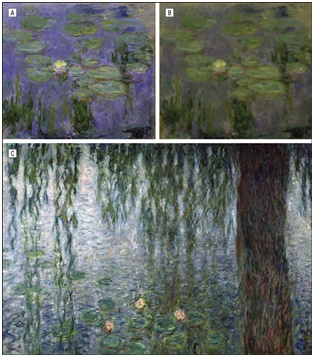
Claude Monet, the father of French Impressionism, developed cataracts in his old age.
A product of the aging process, no one is immune to cataracts – even artists. French Impressionist painter Claude Monet developed cataracts during his later years, though he would eventually have them removed.
This series of images illustrates how Monet’s cataracts affected his work. Image A, from Waterlilies, was painted while Monet had cataracts. Put through a filter, image B shows what this piece looked like to Monet through his cataracts.Image C, Morning with Weeping Willows, was painted after his cataracts were removed. Notice the differences in color and detail before and after undergoing cataract surgery. The first image really speaks to Monet’s talent as a painter, considering what it looked like to him!
With a 98% success rate modern cataract surgery is one of the safest and most effective surgical procedures performed today. There are more than 3 million cataract surgeries performed in the U.S. every year, and most patients experience greatly improved vision after the surgery. Thanks to computer-assisted technology and the femtosecond laser, it is safer than ever to undergo cataract surgery. If you’re experiencing vision loss due to cataracts, speak with your ophthalmologist today about the best treatment options available to you. Enjoy incredible sight for life!
BIO: Hayley Irvin is a graduate of the University of Oklahoma. When she’s not creating awesome content for Marketing Zen Group & Eyecare2020 , she’s writing about basketball, learning about space, and thwarting her cats’ attempts to take over the world. Catch up with her on Twitter @HayleyNIrvin.