Many people think our obsession with cleanliness is to blame for the rise in allergies such as hay fever, eczema and asthma.
The idea is that modern hygiene standards have reduced our exposure to good and bad germs, which can help strengthen the immune system, the body’s mechanism for keeping us healthy.
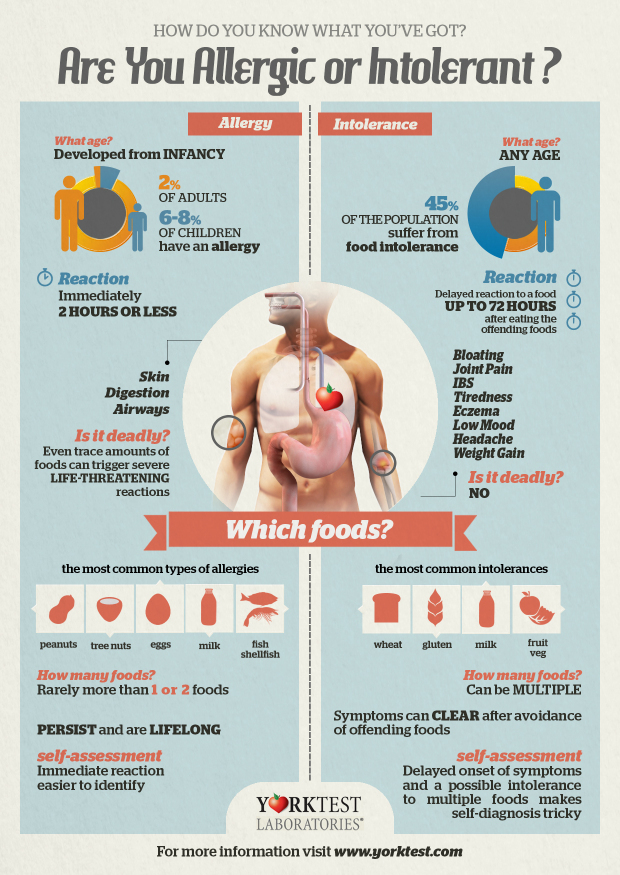
Over the past 20 years there has been a rise in allergies, and no-one really knows why. Around one in four people in the UK suffers from an allergy at some point in their lifetime and numbers are increasing every year.
Research suggests that exposure to germs is only one possible reason for this and diet, lack of exercise, our environment, use of antibiotics and a family history of allergies may play a bigger role.
But what is increasingly clear from the evidence is that hygiene standards should not be relaxed to try to reduce the risk of developing an allergy.
Are we being too clean?
No. It is very important that we maintain good standards of personal and home hygiene.
Good hygiene is about avoiding infection and preventing the spread of infection to others. Good hygiene isn’t about being dirt-free and doesn’t require being obsessively clean. Good hygiene is about preventing the spread of germs at times and in places and situations where it really matters, such as when preparing food, after using the toilet, after sneezing and when someone’s ill with an infection.
Find out how to prevent germs from spreading.
Where did this idea of being ‘too clean’ originate?
The idea is based on “the hygiene hypothesis”, first proposed in a 1989 study by Prof David Strachan, which suggests that a lack of childhood exposure to harmful germs and fewer childhood infections are to blame for the rise in allergies.
Although it is catchy, the phrase “hygiene hypothesis” is somewhat misleading and it has been wrongly used in the media to suggest that modern hygiene standards are bad for our health.
It is important that we do not relax our personal and home hygiene standards. Exposure to germs is only one of several reasons that could explain the rise in allergies and may not be the most important one.
Check an interactive guide on hygiene hypothesis from the International Scientific Forum on Home Hygiene.
Can homes really be ‘too clean’?
No amount of cleaning can rid the home of germs. As fast as they are removed by cleaning, new germs return via humans and pets, contaminated food, the outside air etc. The idea that we now live in sterile homes is totally wrong. It’s impossible to sterilise our homes.
Why is hygiene important?
Good hygiene is critical in stopping the spread of disease-causing germs, such as colds and flu, tummy bugs like campylobacter, salmonella and E. coli O157, in the home and beyond, on food, from our pets and between people. Particular care should be taken to protect at-risk groups such as babies, whose immune systems have not fully developed, and people with a weakened immune system because of illness or medication.
Doesn’t exposure to germs strengthen our immune system?
It is thought that exposure to both good and bad germs in the first few years of life helps to develop the immune system – an idea distinct to the hygiene hypothesis. This helps the body to learn how to fight infection and to tell the difference between harmful and harmless substances.
Throughout life, it is also important that our bodies have the right balance of some exposure to both good and bad germs (present in our everyday environment), particularly in our gut and on our skin, to ensure that the immune system is trained to deal with different kinds of substances. Changes in this balance can cause the immune system to react unpredictably and it may find it difficult to tell when it is being attacked.
Maintaining this balance means not being afraid of getting outside and getting dirty sometimes. However, you should take every precaution to reduce your exposure to harmful germs by ensuring good personal and home hygiene, particularly if you are in an at-risk group.
Exposure to germs such as E.coli, norovirus and the measles virus can be very dangerous and can lead to life-threatening illnesses. These types of infection can cause permanent damage to your body and immune system so it cannot fight infection as well when it is attacked again.
People who maintain a healthy lifestyle tend to have a stronger immune system. Lifestyle factors that can weaken the immune system include drinking too much alcohol, poor diet and stress.
But can’t you develop immunity to germs like salmonella, E. coli, flu and so on?
To a certain extent, yes. Coming into contact with a specific harmful germ such as salmonella or measles will cause the body to respond and make antibodies, which neutralise the germ and protect against that particular germ. But deliberately exposing yourself to such germs is risky because you may become very seriously ill before your body can respond and fight the infection – and if you survive you will only have developed immunity against that particular germ.
This is why we developed vaccines so that we can be exposed to small safe doses of germs such as the flu, the measles virus and so on in a carefully controlled way that gives us protection without making us ill.
So what else could explain the rise in allergies?
Allergies have risen sharply over the past two decades and we’re not entirely sure why. Changes to the types of germs we come into contact with is only one factor among many that may explain this rise. Other factors include changes in diet and eating allergy-causing foods, where we live, a family history of allergy and how physically active we are.
One theory suggests that we have lost touch with a bunch of good germs, known as “old friends”, that humans evolved alongside back in the Stone Age, when our immune system was still developing. How this may have come about isn’t entirely clear, but measures to protect us from harmful germs – such as public sanitation – may have inadvertently cut us off from these good germs, which live in similar environments.
Who are these old friends?
Scientists aren’t entirely sure, but research suggests they include some of the good germs found on the skin, gut and throat area as well as in our outdoor environment, especially the countryside, which may explain why children on farms have less asthma. These old friends are not thought to include harmful germs that spread infectious diseases such as colds, flu, measles, salmonellosis, norovirus etc.
For more information on the old friends theory, read The Hygiene Hypothesis and its implications for home hygiene, lifestyle and public health (International Scientific Forum on Home Hygiene).
Should we therefore be more relaxed about hygiene?
Even good old countryside dirt can contain harmful germs. So, relaxing hygiene would only expose us to “new enemies”, like E. coli O104, not our old friends. That would raise the risk of infectious disease and take us back to the days when lives were short and one in four children died before the age of five.
So are you less likely to develop allergies if you live on a farm?
There is some evidence that children who grow up on farms develop fewer allergies. The theory is that farms (particularly farm animals) increase exposure to different types of good and bad germs, which stimulate the immune system and reduce the risk that someone will develop an allergy.
Are the chemicals in cleaning products linked to the rise in allergies?
No, there is currently no evidence that links the use of household cleaning products, or their ingredients, such as antibacterial agents, to the rise in allergies, such as hay fever and asthma.
Is personal hygiene a likely factor in the rise in allergies?
Bathing and showering does remove germs from our skin but there is no evidence linking frequency of washing, showering or bathing to an increased risk of allergies.
Are antibiotics to blame for the rise in allergies?
There is some evidence linking the use of antibiotics with the rise in allergies. It is thought that antibiotics may reduce the amount of germs on our skin and in our gut. This upsets the body’s normal balance and the immune system finds it difficult to tell the difference between harmless and harmful germs.
Are vaccines to blame for the rise in allergies?
Vaccines are not thought to be associated with rising allergy levels. Vaccination has saved more lives and prevented more serious diseases than any advance in recent medical history.
Vaccines work by stimulating our immune system to produce antibodies (substances produced by the body to fight disease) without actually infecting us with the disease. As with all new medicines, all vaccines are extensively tested for safety before they’re made routinely available to the general public. Find out more about vaccinations.
Are changes in diet to blame for the rise in allergies?
There is some evidence that changes to childhood diets may be responsible for an increase in allergies.
It is thought that introducing foods that can cause an allergy (allergens) such as peanuts, milk and egg during weaning and alongside continued breastfeeding, can reduce the number of children developing allergic disease in later childhood. However, this is only a theory and there are currently a number of studies ongoing around the world that aim to answer this very important question.
Until we know the answer, mothers should continue to follow the current national advice, which is to exclusively breastfeed your baby for around the first six months of their life and not to give them allergenic foods before six months of age, such as peanuts, nuts, seeds, egg, fish, shellfish, milk, soya, wheat (and other cereals that contain gluten such as rye, barley and oats). Find out more about breastfeeding and weaning.